









The antimicrobial resistance (RAM) It is one of the most important global public health problems and different health organizations and governments are increasingly concerned because this situation is increasing. more deaths and medical costs.
The World Health Organization (WHO) estimates that in 2019 5 million lives were lost worldwide as a result of antimicrobial resistance. And at a global conference this week that Infobae covered, experts from the global health entity explained how existing vaccines have the potential to prevent deaths from AMR, and lower the costs of treatments that ultimately do not work.
They did it by announcing a report published last Thursday where they highlight that vaccines have the potential to prevent approximately 515,000 of these deaths each year reducing the incidence of infections, the transmission of pathogens, the use of antibiotics and, subsequently, the evolution of resistance genes.

“The role of vaccines in reducing antimicrobial resistance has been little recognizedbut vaccines have the power training the immune system to mount a defense against various pathogens before the infection starts or becomes serious,” he explained to Infobae Yvan Hutin, director of surveillance, protection and control of the WHO Antimicrobial Resistance Division.
“The best infection is the one that does not occur. “When we vaccinate people, they do not develop infections and do not need antibiotics,” said Hutin, adding that vaccinated people will have fewer infections and, therefore, will also be protected against possible complications of secondary infections that may trigger the use of antimicrobials or require hospitalization. hospitable.
The study presented focuses on 24 pathogens and 44 vaccines (either authorized by regulatory agencies or in clinical development). Some of the vaccines highlighted in the report, such as the pneumococcal conjugate vaccine, which protects against infections by Streptococcus pneumoniaehave existed for years, but are little used. Others, including tuberculosis (TB) vaccine candidates, Escherichia coli and Klebsiella pneumoniaeare still in clinical development.

Combining the knowledge of international experts with data and a solid methodology, the report aims to quantify the potential of these vaccines to reduce antimicrobial resistance, their effects and their antibacterial use. Vaccines against 24 pathogens could reduce the number of antibiotics needed by 22% or 2.5 billion daily doses defined globally each year, as estimated by the WHO, supporting global efforts to address antimicrobial resistance (AMR).
It is estimated that RAM kills more than a million people every year and is associated with almost five million deaths annually. But if these vaccines were widely deployed and included in national and global antimicrobial resistance mitigation strategies, the report concludes, they could dramatically reduce the incidence of infections that drive antibiotic use and create selective pressure for bacteria. drug resistant.
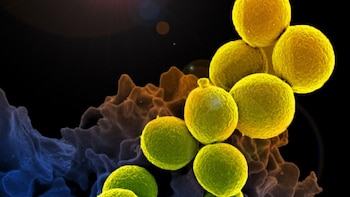
AMR occurs when bacteria, viruses, fungi, and parasites They no longer respond to antimicrobial medications, making people sicker and increasing the risk of illness, death, and the spread of difficult-to-treat infections. Antimicrobial resistance is largely due to the misuse and overuse of antimicrobials; However, at the same time, many people around the world do not have access to essential antimicrobials.

The doctor Mateusz Hasso-Agopsowiczlead author of the report and a WHO technical official, specified that the objective of the report was to quantify the impact that vaccines could have on antimicrobial resistance based on three criteria:
- The health burden related to antimicrobial resistance
- The economic burden (including hospital costs and productivity losses)
- The use of antimicrobials
To do this, the WHO analyzed data and requested expert opinion on 44 different vaccines targeting 24 pathogens (19 bacteria, 4 viruses, and 1 parasite). They began by analyzing the vaccines that already existed against S. pneumoniae, Haemophilus influenzae type b (HIB) and Salmonella Typhi (typhoid fever).
If distributed more widely, they found they could prevent up to 106,000 deaths related to antimicrobial resistance, 9.1 million disability-adjusted life years (DALYs) and $861 million and $5.9 billion in hospital and productivity costs, respectively, while reducing antibiotic use in 142 million defined daily doses (DDD).
“Countries must increase use of existing vaccines. We already have them in our arsenals and we must ensure that we use them appropriately, especially in countries with low vaccination coverage,” said Hasso-Agopsowicz.
The study presented by the experts then examined the potential impact of vaccines in the later stages of clinical development, including vaccine candidates for tuberculosis, E. coli extraintestinal pathogenic (ExPEC), gonorrhea and Salmonella Paratyphi A. The report estimates that if these vaccines were approved and introduced quickly, they could prevent up to 135,000 deaths a year, along with 5 million DALYs, $1.2 billion in hospital costs, and $2.2 billion in lost productivity.

Hasso-Agopsowicz noted that a tuberculosis vaccine alone would dramatically reduce annual antimicrobial use, since treatment regimens for this disease are very long, clocking in at 6 months or more and involving several medications a day.
“If we developed and fully used vaccines [contra la tuberculosis], we could avoid between 1,200 and 1,900 million doses of antimicrobials, which represents a large proportion of the total antimicrobial load,” he highlighted.
Experts also identified early stages of clinical development, such as a maternal vaccine targeting K. pneumoniae, which is the main cause of neonatal sepsis worldwide. Other vaccine candidates in this group target Acinetobacter baumannii, Staphylococcus aureus and Streptococcus from group A.

On the whole, could prevent up to 408,000 deaths, 23 million DALYs, $30 billion in hospital costs, and $17.7 billion in annual productivity losses. They would also reduce antimicrobial use by 548 million DDD. The report points out, however, that although the vaccine candidates in this group have a high potential impact on AMR, the feasibility of the development of some is low due to the difficulties in identifying and accessing the vaccine’s target populations.
“Vaccines are an essential part of the response to reducing antimicrobial resistance, preventing infections, reducing use and overuse of antimicrobials and slow the emergence and spread of drug-resistant pathogens”, remarked Dr. Hutin and highlighted the results of the new report that expands a WHO study published in BMJ Global Health last year.
“Addressing antimicrobial resistance begins with preventing infections, and vaccines are among the most powerful tools to achieve this,” said Dr. Tedros Adhanom Ghebreyesus, Director-General of the WHO, in a post-conference message.
He added: “Prevention is better than cure, and increasing access to existing vaccines and developing new ones for critical diseases, such as tuberculosis, is essential to saving lives and turning the tide on antimicrobial resistance.”

The doctor Martin Friede, of the Department of Immunization, Vaccines and Biological Products of the WHO, indicated that although health experts have known for many years that vaccines could play a role in controlling AMRthe report’s estimates now give vaccine developers and AMR stakeholders a starting point for prioritize research and development efforts.
“So far we have not been able to say which vaccines could play a role [contra la resistencia a los antimicrobianos] and what its impact could really be. Now, with this report, we know how much they can contribute,” said the expert.
The WHO study recommends that global, regional and national antimicrobial resistance and immunization strategies and implementation frameworks include vaccines as interventions to reduce antimicrobial resistance and promote their broader application.

For example, the report calls for global vaccination coverage against S. pneumoniae to achieve the goal of the WHO and the Immunization Agenda for 2023 of 90% in children.
To boost vaccine development, the report recommends including AMR endpoints in clinical trials, collaborating with regulatory agencies, and creating research roadmaps for challenging bacterial vaccines.
“This is a call to action. Governments, the private sector and investors must invest in the development of new and improved vaccines. Robust research and development is really needed to represent a step-change in the fight against the growing threat of antimicrobial resistance,” concluded Dr. Hasso-Agopsowicz.
